POTS Treatment in Melbourne and Online Australia Wide
If you have been diagnosed with POTS, or suspect you may have it, you already know how disruptive it can be.
Standing feels overwhelming. Your heart races. Your head feels foggy. Your energy disappears quickly. You may look fine on the outside, yet internally your system feels unstable and unpredictable.
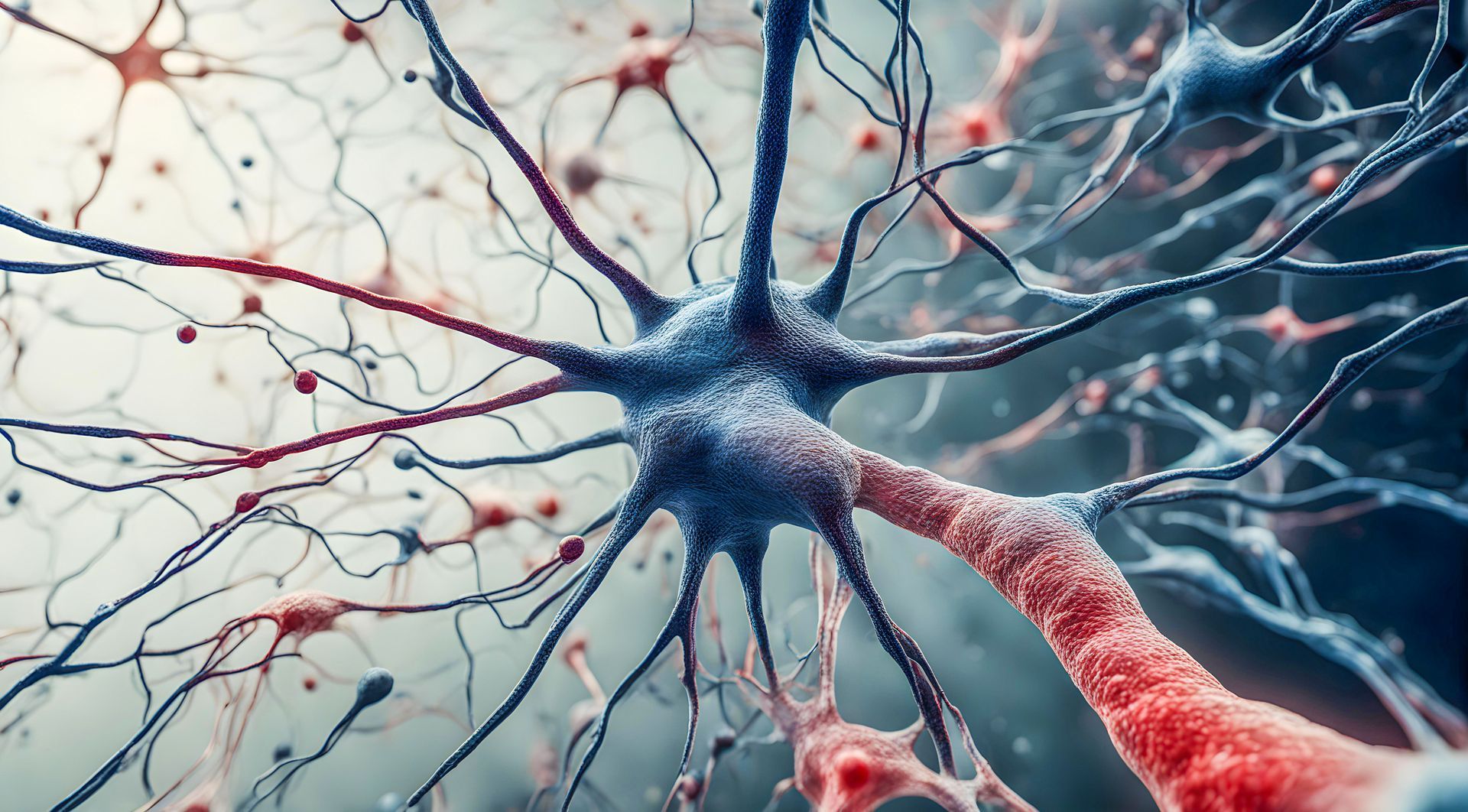
Postural Orthostatic Tachycardia Syndrome, or POTS, is often described as a heart rate condition. Clinically, it involves an increase in heart rate of thirty beats per minute or more within ten minutes of standing. But what I want you to understand is that POTS is fundamentally a nervous system regulation disorder.
Your brain and autonomic nervous system control posture, circulation, balance, energy production and stress responses. When this system becomes dysregulated, standing upright becomes physiologically stressful.
That is where my neurological functional approach comes in.
Why I Focus on the Brain in POTS
Every time you stand, your brain must coordinate blood vessel tone, heart rate, muscle activation and sensory integration in milliseconds. This involves the brainstem, cerebellum, vestibular system and autonomic pathways working together seamlessly.
If that communication is inefficient, your body overcompensates.
Your heart rate spikes. Blood pools in the lower body. You feel dizzy, fatigued or mentally foggy. Over time, your nervous system can remain in a heightened stress pattern.
In my practice, I focus on improving how your brain regulates these systems rather than simply managing symptoms.
Instead of asking how we suppress your tachycardia, I ask how we improve your regulation.
How I Work With POTS
My neurological functional method is designed to strengthen and retrain specific neural pathways involved in posture, circulation and autonomic balance.
Depending on your presentation, your program may include:
• Targeted neurological stimulation
• Vestibular and balance integration
• Postural retraining
• Sensory integration strategies
• Graduated movement progressions to build upright tolerance
• Structured pacing to reduce flare cycles
Everything is personalised. I do not push you beyond what your nervous system can adapt to. The goal is progressive regulation, not exhaustion.
As your system becomes more efficient at processing sensory input and coordinating vascular responses, many patients report improvements in stamina, mental clarity and resilience.
Common POTS Symptoms I See in Clinic
POTS is rarely just one symptom. It often presents with:
• Rapid heart rate on standing
• Dizziness or light headedness
• Brain fog
• Fatigue and exercise intolerance
• Temperature sensitivity
• Digestive irregularities
• Internal shakiness or anxiety
Because POTS affects multiple systems, an integrated neurological approach is often more effective than addressing each symptom in isolation.
POTS and Long Covid
There has been a significant rise in POTS following viral infections, including long covid. In many cases, the virus acts as a stressor that disrupts autonomic regulation. The nervous system remains in a maladaptive state even after the acute infection resolves.
Supporting nervous system integration and autonomic balance can be particularly important in these cases.
Can POTS Improve
Yes, many people experience meaningful improvement when the nervous system is supported appropriately. Progress requires structure, consistency and individualised pacing.
This is not about forcing your body to tolerate stress. It is about retraining your system so standing, moving and living feel stable again.
Work With Me
If you are searching for POTS treatment in Melbourne, or looking for a neurological approach to POTS online in Australia or worldwide, I can help.
I offer:
•
Face to face sessions in Melbourne
• Online consultations across Australia
• Online sessions worldwide
If you are ready to move beyond symptom chasing and focus on restoring regulation, I invite you to book a session at www.drtonybriggs.com
Your nervous system can adapt. It just needs the right input.
Book your consultation today and let us begin the process of rebuilding stability, clarity and resilience.
Referances
- Raj S R. Postural Tachycardia Syndrome. Circulation. 2013;127:2336 to 2342.
- Sheldon R S et al. 2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of Postural Tachycardia Syndrome. Heart Rhythm. 2015;12:e41 to e63.
- Arnold A C et al. Postural Tachycardia Syndrome Mechanisms and Management. Journal of the American College of Cardiology. 2018;72:1883 to 1896.
- Vernino S et al. Autonomic Disorders. Continuum. 2020;26:44 to 68.
- Freeman R et al. Consensus Statement on the Definition of Orthostatic Hypotension and Related Disorders. Clinical Autonomic Research. 2011;21:69 to 72.